Diagnostic Tests for Cerebral Palsy
Whether a child is diagnosed with cerebral palsy shortly after birth or later in childhood, a number of diagnostic tests and screenings can help predict or explain the birth injury. The physical examinations, lab tests, and medical evaluations available to families with an injured child can provide insight into the severity of the birth injury, how and when it occurred, and the necessary interventions to minimize its associated handicaps. In this section, we’ll discuss how Apgar scores, brain imaging, umbilical cord blood tests, and other diagnostic tests for cerebral palsy work.
We encourage the family members and friends of children with birth injuries to reach out to our lawyers with their legal questions. Our Detroit, Michigan birth injury attorneys will provide you with a free case review and determine whether medical malpractice caused your loved one’s birth injuries. You may call Michigan Cerebral Palsy Attorneys toll-free at (888) 592-1857, press the Live Chat tab to the left, fill out this contact form, or press the contact button below.
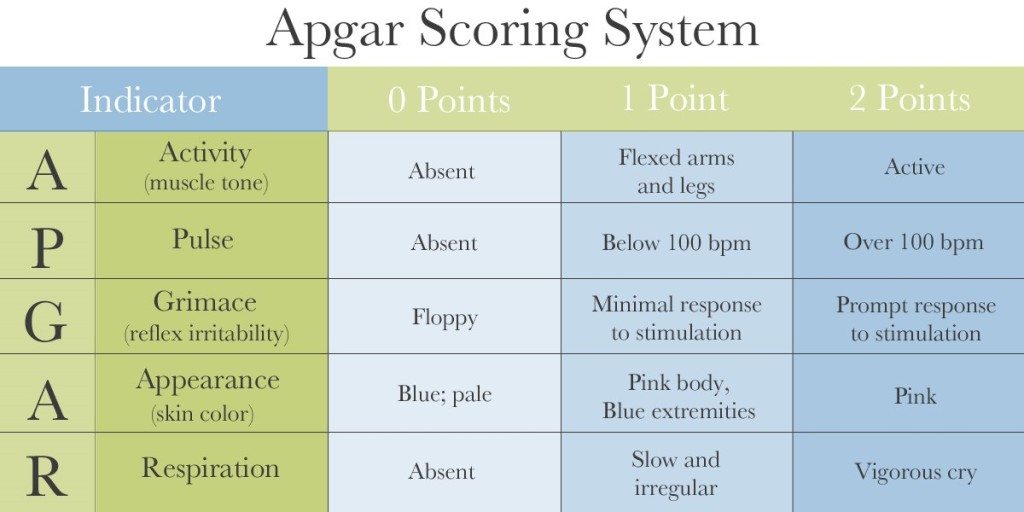
1. Apgar Score
For over 60 years the Apgar score had been used to quickly and simply assess the health of a baby immediately after delivery and predict survival. Typically conducted from one to five minutes after birth, the Apgar score evaluates the baby on the five following criteria:
- Appearance/complexion:
- Score of 0: The baby is entirely blue or pale
- Score of 1: The baby is blue in the extremities or has a pink body
- Score of 2: The baby has no abnormal coloring; the baby is pink in the body and extremities.
- Pulse rate:
- Score of 0: The baby’s heart rate is absent
- Score of 1: The baby’s heart rate is slow (less than 100 beats per minute/BPM)
- Score of 2: The baby’s heart rate is fast (greater than 100 BPM)
- Reflex irritability (grimace):
- Score of 0: The baby has no response to stimulation
- Score of 1: The baby responds to stimulation by grimacing and crying
- Score of 2: The baby cries and pulls away when stimulated
- Activity:
- Score of 0: The baby exhibits no activity
- Score of 1: The baby has some flexion (joint movement)
- Score of 2: The baby has flexed arms and legs that resist extension
- Respiratory effort:
- Score of 0: The baby does not breathe
- Score of 1: The baby has weak, irregular, or gasping breaths
- Score of 2: The baby has a strong cry
Below is a visual representation of the Apgar scoring chart:
The physician scores the baby from 0 to 2 on each criterion, and then the doctor adds the sum of the five values to determine the final score. Scores of 1-3 are critically low, 4-6 are below normal, and 7+ are normal. Low scores indicate that the baby has a higher chance of needing medical interventions like resuscitation. If the score remains low for longer time intervals (such as 10, 15, or 30 minutes after birth), the child is at risk for suffering long-term neurological damage.
It is crucial to remember that high Apgar scores do not rule out the possibility of brain injuries like cerebral palsy and HIE. Apgar scores are not devised to make long-term predictions regarding the baby’s health.
2. Brain Imaging Tests
A cerebral palsy diagnosis is typically based on the child’s history and physical examination. Once a child is diagnosed with cerebral palsy, further brain imaging tests can reveal the cause, timing, and severity of the initial brain damage. Abnormal neuroimaging studies indicate a greater likelihood of associated complications and conditions such as epilepsy, cognitive delays, and developmental disabilities. Regardless of when the diagnosis is made, brain imaging results can help predict or explain a birth injury.
Once signs of cerebral palsy or hypoxic ischemic encephalopathy are observed, the following brain imaging tests and studies are conducted to diagnose cerebral palsy:
- MRI: Magnetic Resonance Imaging (MRI) tests uses magnetic waves to make pictures of structures inside the baby’s brain. MRIs are the best imaging technique for HIE diagnosis and can be performed as early as 12 hours after birth. MRIs take images of the brain that make lesions visible.
- Ultrasound: Cranial ultrasounds use sound waves to evaluate blood flow in the vessels going to the brain or within the brain. While ultrasounds have low sensitivity for detecting HIE, their readings have high sensitivity for showing hemorrhages and ventricular size.
- CT scan: CT scans use X-rays and computer software to make pictures of the baby’s brain.
- EEG (electroencephalogram): EEGs record the activity of the baby’s brain by measuring electrical currents through the brain. EEG tests are crucial when seizure activity is possible—in newborn babies, seizures often have no visible indicators and can cause severe brain damage when left undiagnosed or undetected.
- Evoked potential test: Evoked potential tests are neurophysiological tests that evaluate the functioning of the baby’s brain by recording brain waves.
3. Umbilical cord blood gas tests
Physicians can determine whether a baby has suffered an oxygen-depriving insult (referred to as an anoxic or hypoxic-ischemic event) by examining blood from the umbilical artery. Umbilical cord blood reveals information about the baby’s experience because it is blood that comes directly from the fetus (as opposed to blood that goes to the fetus from the mother).
Physicians are able to test umbilical cord blood tissues for acidity to determine if the baby suffered oxygen deprivation during the pregnancy or delivery. If the cord blood contains high levels of acid it is considered “acidemic.” Acidemic umbilical cord blood usually reveals that a process known as “anaerobic metabolism” occurred, which is a form of metabolism that occurs when oxygen isn’t available. Anaerobic metabolism results in anoxic or hypoxic-ischemic events which cause hypoxic ischemic encephalopathy (brain damage caused by limited oxygen) and ultimately cause cerebral palsy and seizure disorders.
Legal Help for Families Affected by HIE, Cerebral Palsy, or Other Birth Injuries
The Michigan Cerebral Palsy Attorneys have decades of experience providing legal support to the families emotionally and financially burdened by a birth injury. Whether your loved one’s cerebral palsy resulted from a mishandled diagnosis or from another negligent medical handling of a birth injury, we’re here to help. Call us today at (888) 592-1857 and we will review your loved one’s case for free and answer any of your legal questions.
Sources:
- Yeh, P., Emary, K., & Impey, L. (2012). The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51 519 consecutive validated samples. BJOG: An International Journal of Obstetrics & Gynaecology, 119(7), 824-831.
- Malin, G. L., Morris, R. K., & Khan, K. S. (2010). Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ: British Medical Journal, 340.
- ACOG Committee on Obstetric Practice. ACOG Committee Opinion No. 348, November 2006: Umbilical cord blood gas and acid-base analysis. Obstet Gynecol 2006; 108:1319.
- Armstrong L, Stenson BJ. Use of umbilical cord blood gas analysis in the assessment of the newborn. Arch Dis Child Fetal Neonatal Ed 2007; 92:F430.
- Nageotte, MP, Gilstrap, LC III. Intrapartum fetal surveillance. In: Creasy & Resnik’s Maternal-Fetal Medicine Principles and Practice, 6th ed, Creasy, Resnik, Iams, Lockwood, Moore (Eds), Saunders, Philadelphia, PA 2009. p.397.
- Page FO, Martin JN, Palmer SM, et al. Correlation of neonatal acid-base status with Apgar scores and fetal heart rate tracings. Am J Obstet Gynecol 1986; 154:1306.